Utilize our thrombocytopenia calculator for quick assessments. Simplify platelet count analysis for informed medical decisions with ease and accuracy.
RESULTS
Navigating the complexities of thrombocytopenia can be daunting for both patients and healthcare providers alike. Thrombocytopenia, a condition characterized by abnormally low platelet counts, has various causes that require careful evaluation.
This guide will help you to use a Thrombocytopenia Calculator as an effective tool in assessing the risk of heparin-induced thrombocytopenia (HIT), helping you interpret results with confidence.
Understanding Thrombocytopenia
Thrombocytopenia isn’t just a challenge for healthcare providers—it’s a puzzle where every piece matters, from the platelets in our blood to the diverse causes behind their decline.
Definition
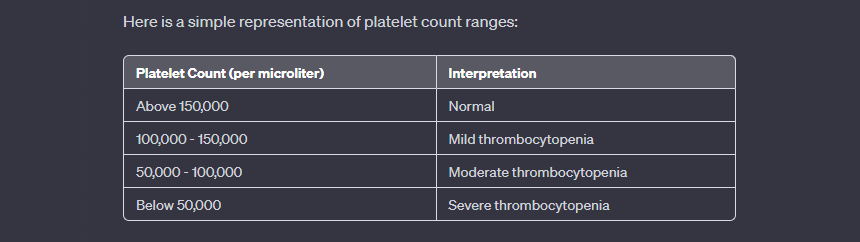
Thrombocytopenia is when you have too few platelets in your blood. Platelets help stop bleeding by clumping and forming plugs in blood vessel injuries. If you don’t have enough, it can cause excessive bleeding and easy bruising.
This condition can happen for different reasons, such as side effects from medicines, viral infections, autoimmune diseases, or genetic issues. It’s really important to find out why someone has low platelets so they can get the right treatment.
Causes
Now that you know what thrombocytopenia is, let’s talk about why it happens. Your body might not make enough platelets if you have certain conditions, like leukemia, or if your bone marrow isn’t working right.
Sometimes, though, your body might break down platelets too fast. This can happen with autoimmune diseases, where the body attacks itself by mistake. Infections and some medicines are also known to lower platelet counts.
Genetic factors play a role too. If you inherit a platelet disorder from your family, it could lead to low platelet counts. Liver problems or heavy alcohol use can affect how your blood clots because they change how your liver makes clotting factors and cleans the blood of toxins, which are bad for platelets.
Cancer and its treatments often harm bone marrow as well, reducing the number of healthy blood cells produced, including platelets. Also, try our Blood Type Calculator, it’s a fun way to explore your blood type and its implications.
Heparin-induced thrombocytopenia (HIT)
Heparin-induced thrombocytopenia, or HIT, is a complex and potentially life-threatening adverse reaction to heparin treatment. Characterized by an immunological response leading to reduced platelet counts, it poses significant risks for patients—prompting the need for swift and accurate diagnosis through clinical scoring systems such as the 4Ts score.
What is HIT?
HIT is short for Heparin-Induced Thrombocytopenia. It’s a problem that can happen when someone takes the blood thinner heparin. This medicine usually stops blood clots from forming, but sometimes it causes a low platelet count.
That makes clotting even more likely, which can be dangerous.
Doctors look out for HIT by using things like the Thrombocytopenia Calculator. They use this tool to figure out if someone could get HIT. It helps make sure they catch it early and treat it right away to prevent serious problems.
Healthcare providers rely on it to make smart choices about how to help their patients safely.
4Ts Score for HIT
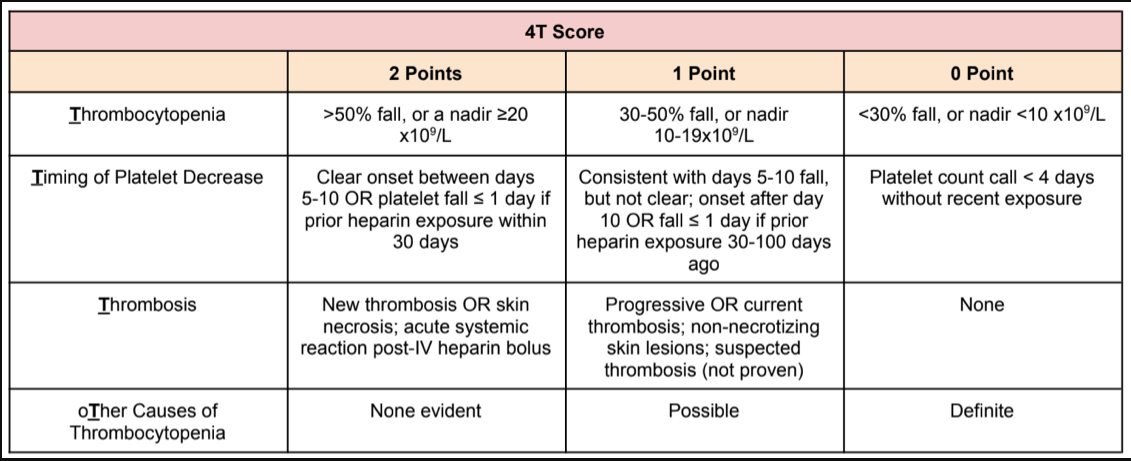
Doctors use the 4Ts Score to figure out if a patient might have HIT. This score checks how low the platelet count is, when the drop happened after using heparin if there are any blood clots or skin reactions, and if something else could be causing the low platelets.
A higher total score means HIT is more likely. With this tool, doctors can decide if they need to do more tests like the HIT antibody test. It guides them in treating patients correctly and avoiding steps that aren’t needed.
Calculating the 4T score helps avoid overdiagnosis and gives patients better care. Let’s learn how to calculate it with the precise steps below. Also, try our Reticulocyte Calculator, and delve into your reticulocyte count for insights into your overall blood health.
Step-by-step Guide On How To Use Our Calculator
Select “Thrombocytopenia” Option: Choose “Thrombocytopenia” on the calculator to assess platelet count changes and nadirs. Opt for “Platelet count fall >50% AND platelet nadir ≥20” if it matches your situation.
Fill in Details: Answer questions about platelet drop timing, clotting, and potential causes. Be precise with your health information.
Click Calculate: After entering details, press “Calculate” to determine the likelihood of heparin-induced thrombocytopenia (HIT). Results include points and HIT probability.
Assess Platelet Fall 30–50% OR Platelet Nadir 10–19: If platelet count drops or reaches a low, input the numbers for severity assessment. Crucial for understanding thrombocytopenia severity.
Consider Prior Heparin Exposure within 30 Days: Check if heparin was used in the last month. The calculator factors this for spotting possible heparin-induced issues.
Evaluate Consistent Platelet Fall with Days 5–10, But Not Clear; Onset After Day 10 OR Fall ≤1 Day: Address uncertain platelet drop timing. Include heparin use from 30 to 100 days ago. The calculator helps assess the likelihood of HIT.
Analyze Platelet Fall <4 Days Without Recent Exposure: If the platelet count drops quickly, assess the risk of clotting problems. Look for signs of ongoing or recurrent clots and skin issues.
Choose the “Not Proven” Option: Understand the calculator doesn’t cause thrombocytopenia. It aids in predicting the likelihood of heparin-induced thrombocytopenia (HIT).
Select “None” for Thrombosis or Other Sequelae: Choosing “None” suggests no new clots or skin reactions after heparin, possibly indicating HIT may not be an issue.
Evaluate New Thrombosis OR Skin Necrosis; Acute Systemic Reaction Post-IV Heparin Bolus: Consider signs of new blood clots or skin issues post-IV heparin. Assess for other possible causes for low platelets.
Consider “Possible” for Other Causes for Thrombocytopenia: If no clear cause, consider factors contributing to platelet decrease. This aids in understanding potential causes and assessing HIT likelihood.
Choose “Definite” for Other Causes for Thrombocytopenia: If sure another cause is to blame, select “Definite.” Press “Calculate” to obtain HIT probability and points based on evidence.
Hit Calculate for Final Results: After completing the steps, click “Calculate.” The tool provides scores and probability for HIT, aiding healthcare decisions.
Example
Let’s say Sarah has a sudden drop in platelets after receiving heparin. Her doctor uses our calculator to see if she might have HIT. They selected “Platelet count fall >50% AND platelet nadir ≥20” because her platelets went from 300,000/μL to 100,000/μL.
For timing, they chose “Clear onset between days 5–10” as it fits her case. Sarah had no other signs of thrombosis and no obvious other cause for the low platelets. So, her doctor clicks “None apparent.” After hitting calculate, the results show Sarah’s likelihood of having HIT.
Imagine another patient, John, who also received heparin recently but has different symptoms. His platelets dropped a bit less—from 250,000/μL to 130,000/μL—and his lowest count was around day four with no prior exposure in the last month.
The doctor picks options that match John’s situation and calculates again. This time, the results help guide what steps to take next for John’s care.
FAQs
1. Can this calculator tell if I might have disseminated intravascular coagulation (DIC)?
Sure can—it’s smart like that! The calculator looks at all sorts of data to help doctors decide if DIC might be the culprit messing with your body’s ability to form clots properly.
2. How accurate are these calculators when predicting conditions linked to low platelets?
Well, they’re pretty on point most time! These calculators use smarty-pants math equations—and we’re talking positive predictive value here—to make educated guesses about your health condition based on numbers from folks just like you.
3. Do I need special medical knowledge to understand the results of a thrombocytopenia calculator?
Not really! While terms like ECMO or MSD may sound techy-techy, your doctor will break it down for you into plain talk—you’ll know exactly what those numbers mean for your basal metabolic rate or anything else they measure.
4. Can the Thrombocytopenia Calculator be used for self-diagnosis?
No, it’s meant for healthcare professionals only.
5. How often should platelet counts be monitored for someone with thrombocytopenia?
Doctors decide based on each person’s situation; there is no one rule.
6. Does heparin use always lead to HIT?
Not always; HIT occurs in some people who receive heparin treatment, but not all.
7. Who can get thrombocytopenia?
Anyone can get it but certain illnesses or treatments like chemotherapy raise your risk.
8. Is D-dimer testing useful in diagnosing HIT?
D-dimer levels may rise in HIT, but this test alone isn’t enough to diagnose it.
Related Calculators: